Health
New imaging technique allows researchers to see gene expression in brains of live mice in real time
A University of Minnesota Twin Cities-led team has developed a new technique that allows scientists and engineers to, for the first time, visualize mRNA molecules in the brains of living mice. The research reveals new insights into how memories are formed and stored in the brain and could provide scientists with new information about diseases such as Alzheimer’s.
The paper is published in the Proceedings of the National Academy of Sciences of the United States of America (PNAS), a peer-reviewed, multidisciplinary, high-impact scientific journal.
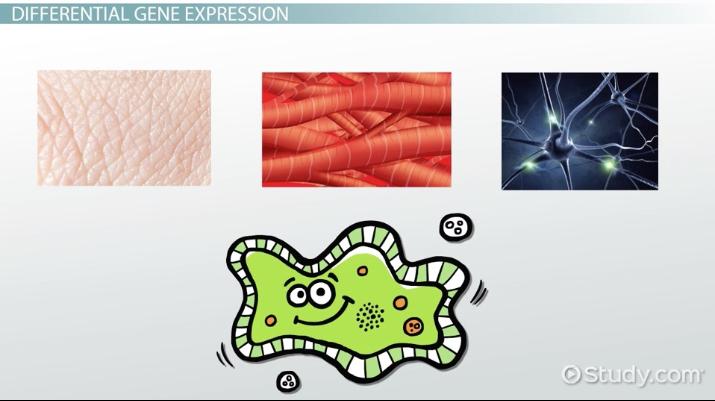
There is still a lot of mystery surrounding the process of how memory is physically created and stored in the brain. It is well known that mRNA—a type of RNA involved in the creation of proteins—is produced during the process of forming and storing memories, but the technology for studying this process on the cellular level has been limited. Previous studies have often involved dissecting mice in order to examine their brains.
A team of researchers led by a University of Minnesota Twin Cities faculty member has developed a new technique that gives scientists a window into RNA synthesis in the brain of a mouse while it is still alive.
“We still know very little about memories in the brain,” explained Hye Yoon Park, an associate professor in the University of Minnesota Department of Electrical and Computer Engineering and the study’s lead author. “It’s well known that mRNA synthesis is important for memory, but it was never possible to image this in a live brain. Our work is an important contribution to this field. We now have this new technology that neurobiologists can use for various different experiments and memory tests in the future.”
The University of Minnesota-led team’s process involved genetic engineering, two-photon excitation microscopy, and optimized image processing software. By genetically modifying a mouse so that it produced mRNA labeled with green fluorescent proteins (proteins derived from a jellyfish), the researchers were able to see when and where the mouse’s brain generated Arc mRNA, the specific type of molecule they were looking for.
Because the mouse is alive, the researchers could study it for longer periods of time. Using this new process, the researchers performed two experiments on the mouse in which they were able to see in real time over a month what the neurons—or nerve cells—were doing as the mouse was forming and storing memories.
Historically, neuroscientists have theorized that certain groups of neurons in the brain fire when a memory is formed, and that those same cells fire again when that moment or event is remembered. However, in both experiments, the researchers found that different groups of neurons fired each day they triggered the memory in the mouse.
Over the course of several days after the mouse created this memory, they were able to locate a small group of cells that overlapped, or consistently generated the Arc mRNA each day, in the retrosplenial cortex (RSC) region of the brain, a group which they believe is responsible for the long-term storage of that memory.
“Our research is about memory generation and retrieval,” Park said. “If we can understand how this happens, it will be very helpful for us in understanding Alzheimer’s disease and other memory-related diseases. Maybe people with Alzheimer’s disease still store the memories somewhere—they just can’t retrieve them. So in the very long-term, perhaps this research can help us overcome these diseases.”
This research was funded by the Samsung Science and Technology Foundation and the Wellcome Trust.
In addition to Park, the team included Seoul National University researchers Byung Hun Lee, Jae Youn Shim, Hyungseok Moon, and Dong Wook Kim; and Korea Institute of Science and Technology researchers Jiwon Kim, Jang Soo Yook, and Jinhyun Kim.
Health
Unlocking Wellhealth Ayurvedic Health Tips: Your Comprehensive Guide to Ayurvedic Bliss

Wellhealth Ayurvedic Health Tips is an old Indian system of natural medicine that can take you on a path to complete health. Ayurveda is a system of medicine that seeks to promote wholeness by means of individualised rituals and practices grounded in ancient knowledge.
Importance of WellHealth Ayurvedic Practices
Discover the rich history of Ayurveda and its all-encompassing approach to health as you delve into its holistic method.
Key Principles of Ayurveda
Learn the secrets of Ayurvedic principles, such as the importance of balance and the ever-changing relationship between the doshas, dhatus, and malas.
Ayurvedic Nutrition and Diet
Learn how the Ayurvedic concept of digestive fire (Agni) is central to healthy eating and how to follow a diet specifically designed for your dosha.
WellHealth Ayurvedic Lifestyle
Practice the seasonal adjustments (Ritucharya) and daily habits (Dinacharya) that help you live a balanced and peaceful existence.
Herbal Remedies for Well-Being
Discover the fascinating world of Ayurvedic herbs and the many ways they may improve your health.
Yoga and Exercise in Ayurveda
Achieve a state of harmonious mind-body functioning via physical exercise that is in tune with your dosha.
Learn Ayurvedic methods for reducing stress and improving mental health via practices like meditation and mindfulness.
Managing Stress and Mental Well-Being
Learn holistic, all-natural Ayurvedic skincare techniques that bring forth your inner light so you may radiate from the inside out.
Beauty and Skin Care in Ayurveda
To ensure pleasant and refreshing sleep, make your bedroom a sleep-friendly place and look into natural remedies for insomnia.
Ayurvedic Practices for Better Sleep
Learn about natural treatments for a variety of digestive diseases and how to improve digestion with Ayurvedic practices.
Digestive Health with Ayurveda
Discover the Ayurvedic methods and medicines that strengthen the immune system and promote well-being.
Ayurveda and Immunity Boosting
Learn about natural therapies for menstruation health and Ayurvedic methods for hormone balance.
Ayurveda for Women’s Health
Start your children out on the right foot by incorporating Ayurvedic principles into their daily lives.
Ayurvedic Practices for Children
Learn the rejuvenation techniques (Rasayana) and some useful pointers for keeping your energy up as you get older.
Ayurveda and Aging Gracefully
Make sure everyone has a good grasp of Ayurveda by clearing up common misconceptions and facts.
The Future of Ayurvedic Wellness
A future where holistic well-being is the foundation of healthcare is becoming more feasible as Ayurveda obtains worldwide reputation and is integrated with contemporary medicine.
Conclusion
Ayurvedic principles can help you live a balanced and healthy life. Ayurveda provides an age-old, all-encompassing method of health care, from individualised diet plans to rejuvenation treatments.
FAQs about WellHealth Ayurvedic Health Tips
What is Ayurveda, and how does it contribute to well-being?
Holistic health is the goal of Ayurveda, an old Indian medical system that emphasises harmony between the physical, mental, and spiritual aspects of a person’s life. It seeks to establish peace and avoid sickness via personalised practices.
How can Ayurvedic nutrition benefit different dosha types?
Because every person has a different constitution, Ayurvedic nutrition takes this into account while designing meals. This method takes into account individual health concerns while encouraging equilibrium.
Is Ayurveda only about herbal remedies, or does it include other practices?
Adjustments to one’s way of life, yoga, meditation, and individualised routines are all part of Ayurveda, which relies heavily on herbal medicines.
Can Ayurveda be integrated with modern medicine?
Ayurveda is a complementary practice to conventional medicine. Comprehensive health benefits can be achieved through integrative techniques that blend Ayurvedic traditions with mainstream therapy.
Are Ayurvedic practices safe for children?
By incorporating Ayurvedic principles into children’s routines, we may start supporting their health at an early age. For specific recommendations, though, it’s best to talk to doctors.
How can Ayurveda contribute to aging gracefully?
By preserving energy and fostering total well-being, rejuvenation treatments (Rasayana) in Ayurveda, in conjunction with lifestyle modifications, facilitate graceful ageing.
Health
Unlock Wellness: 10 Wellhealthorganic Home Remedies Tag

Check out our all-inclusive guide to Wellhealthorganic Home Remedies Tag to discover their potency. Learn about natural ways to live a healthy lifestyle, supported by the knowledge of experts and your own experiences.
Introduction
Taking the first steps towards complete health? Dive into the world of natural health and organic home remedies, where advice from experts meets the healing power of nature. Here we will take a look at ten powerful cures, discussing their uses and the experiences that have made them vital. Let’s start a journey towards better health side by side.
Wellhealthorganic Home Remedies Tag: Unveiling the Power Within
When you shop for home remedies with the Wellhealthorganic tag, you’re getting more than just a label; you’re getting a symbol of the life-changing potential of all-natural products. Delve into the essence of this category and discover a realm where health meets natural cures, resulting in a balanced approach to better living.
The Healing Power of Herbal Teas
Unraveling the Essence
Immerse yourself in the calming realm of herbal teas, where ginger, peppermint, and chamomile become companions on your path to wellness. You may turn to these teas as a treatment for a variety of diseases since they are high in antioxidants and have anti-inflammatory qualities. Revitalise yourself with a sip.
Holistic Nutrition: Nourishing Your Body from Within
Crafting a Nutrient-Rich Plate
Learn about holistic nutrition, the practice that places an emphasis on eating entire foods. Find out how strengthening your body, improving your health, and giving you prolonged energy may be achieved by include organic fruits, vegetables, and superfoods in your diet. From food to energy, it’s all on your plate.
Mindful Meditation: Cultivating Inner Harmony
A Journey Within
Discover the healing power of attentive meditation and escape the maelstrom of everyday life. Devote yourself to a routine that improves your health, decreases stress, and fosters mental clarity. Discover the calmness that comes from being present in the here and now.
Essential Oils: Nature’s Aromatherapy
Harnessing the Essence
Enter the scented realm of essential oils and meet your new best friends: tea tree, lavender, and eucalyptus. Find out how these oils may improve your health and make you feel more refreshed with their relaxing and antibacterial qualities.
DIY Herbal Remedies: Nature’s Apothecary
Crafting Wellness at Home
Make your home a wellness sanctuary by releasing the power of natural treatments you can make at home. Learn to make your own natural medicines that are perfect for your health and wellness, whether that’s an immune-boosting tonic or a skin-soothing balm.
Yoga and Wellbeing: Embracing Harmony
Uniting Body and Soul
Join the yoga practice for a path to inner and outer peace. Gain an understanding of the interconnected nature of mindfulness, asana, and pranayama for a more complete health practice. Find out how yoga can completely change your health journey.
Healing Through Hydrotherapy
Embracing the Waters
Immerse yourself in the healing realm of hydrotherapy, where water serves as a rejuvenating and healing force. Learn how heat and cold therapies may help alleviate pain, increase blood flow, and revitalise you.
Connecting with Nature: The Outdoor Prescription
Nature’s Remedy
Get out into nature and feel its restorative power. Learn about the many ways that going outside, even in a little space like your backyard or a park, may improve your emotional and physical health. Get ready to experience the healing power of nature.
Conclusion
With these game-changing treatments in your arsenal, go out on your wellhealthorganic quest. Discover the many gifts of nature, from herbal drinks to the practice of attentive meditation. Experience the transformative power of wellhealthorganic home remedies tag for your whole health.
Frequently Asked Questions (FAQs)
Q: Can I combine multiple remedies for enhanced benefits?
Sure thing! To achieve a more comprehensive state of health, many people who are passionate about wellhealthorganic combine meditation with herbal beverages and essential oils.
Q: Are these remedies suitable for all ages?
While the majority of cures are perfectly safe for people of all ages, it is always wise to check with a doctor before using any on a youngster, pregnant woman, or someone with a serious medical condition.
Q: How long does it take to experience the benefits of these remedies?
Results may vary, but you should expect to see improvements after a few weeks of regularly using these cures.
Q: Can I replace prescribed medications with wellhealthorganic remedies?
Although these cures can help in a natural way, it is important to talk to your doctor before you modify any of your prescriptions.
Q: Are there any contraindications for these remedies?
Certain herbs or practices may cause reactions in some people. If you are aware of any allergies or pre-existing problems, it is highly recommended that you consult with a healthcare practitioner.
Q: How can I incorporate yoga into my daily routine?
Begin with brief sessions and progressively lengthen them. Beginners might benefit greatly from online sessions or local studios, since they provide sufficient instruction.
Health
Unlocking Well Health Tips in Hindi WellHealthOrganic

Discover a comprehensive approach to Well Health Tips in Hindi WellHealthOrganic with organic recommendations in Hindi—an SEO meta-description. Integrating traditional knowledge with cutting-edge techniques, discover the key to a full, rich existence. For your health journey, dive into professional guidance, frequently asked questions, and practical insights.
Introduction
Being healthy is more than just not being sick; it’s an ever-changing condition of complete mental, emotional, and social fulfilment. Here in this all-inclusive book, we delve into WellHealthOrganic’s Hindi health advice, which combine age-old knowledge with modern methods to help you live a peaceful existence.
The Basics of Well Health
Understanding Well Health
For optimal health, it’s important to consider the whole person, including their thoughts, emotions, and environment. The pursuit of harmony and vigour is an ongoing process, not an endpoint.
Incorporating Organic Practices
Chemical-free, all-natural lifestyles are highly valued according to WellHealthOrganic ideals. An organic lifestyle, including all of your food and personal care items, is beneficial to your health.
Nutrition and Diet
Balanced Diets for Well Health
Maintaining good health begins with eating a balanced diet. Learn why it’s so important to maintain good health by eating a varied diet rich in minerals and vitamins.
Benefits of Organic Food
Learn about all the ways that eating organic foods may improve your health. Choosing organic products has several benefits for your health and the health of the earth, including helping local farmers and lowering your carbon footprint.
Exercise Regimen
Tailoring Workouts for Well Health
Exercise is essential for good health. Mastering the art of individualised exercise plans can help you achieve your fitness goals without putting undue stress on your body.
Embracing Yoga and Meditation
To achieve optimal health in all aspects of life, try using the age-old techniques of yoga and meditation. Practice being present, adaptable, and resilient mentally.
Sleep Hygiene
Importance of Quality Sleep
Getting a good night’s sleep is crucial to your health. Find out how to get a good night’s sleep by solving typical sleep problems, so you can wake up feeling refreshed.
Tips for a Good Night’s Sleep
How to improve your sleep hygiene with simple routines and advice. For maximum health, establish a relaxing nighttime regimen and alter your sleeping habits.
Stress Management
Impact of Stress on Well Health
Negative effects on health can result from stress. Learn how it affects you and look into ways to handle stress well so you may live a balanced life.
Effective Stress-Relief Techniques
Learn a variety of stress-reduction methods, including relaxation exercises and mindfulness practices, to help you face life’s obstacles with grace and strength.
Hydration Practices
Significance of Hydration
Staying well hydrated is essential for good health. Learn how being hydrated may improve your overall vitality and why it’s so important.
Choosing WellHealthOrganic Beverages
To satisfy your thirst and provide your body with nutrients, try some of the delicious and healthy WellHealthOrganic beverage alternatives.
Natural Remedies
Herbal Solutions for Well Health
Harness the medicinal properties of plants. Discover the power of herbal medicines that can enhance your health without the side effects of conventional drugs.
Ayurvedic Practices
Explore the age-old knowledge of Ayurveda. Learn how to improve your health in a way that is specific to your body type.
Immune System Boosters
Foods that Boost Immunity
Consume a diet abundant in nutrients that strengthen the immune system. To strengthen your body’s defences, investigate the nutritional heroes.
Lifestyle Choices for a Strong Immune System
When it comes to immunological health, lifestyle decisions are just as important as food. For long-term health, make changes that strengthen your immune system.
Holistic Well-being
Integrating Physical and Mental Well-being
When a person is truly healthy, they are mentally and physically fit. To live in harmony, one must learn to recognise the unity of mind and body.
Finding Balance in Life
To be healthy, one must find a middle ground in all areas of life. Learn some simple tricks to bring harmony to your day-to-day activities.
Well Health at Work
Tips for a Healthy Workplace
Here are some practical ideas to help you stay healthy while working, even if you have a sedentary job.
Incorporating Wellness into Daily Work Life
Work health and wellbeing into your daily schedule. You may enhance your general well-being by making little modifications.
Mindful Eating
Benefits of Mindful Eating
The nutritional benefits of mindful eating are only the tip of the iceberg. Learn about the life-changing effects of practicing mindful eating.
How to Practice Mindful Eating
Guidelines for making mindful eating a regular part of your routine. Eat more mindfully to improve your health and your relationship with food.
Sustainable Living
Eco-Friendly Practices for Well Health
The state of our planet is a reflection of our overall health. Adopt eco-friendly lifestyle habits that are good for you and the planet.
WellHealthOrganic Living
Find out how to live a WellHealthOrganic lifestyle. Make a commitment to living a healthier, more environmentally friendly lifestyle by making sustainable choices and practicing mindful consumerism.
Family Health Tips
Promoting Well-being in the Family
Promote health and wellness in your household. Here you will find family-focused advice on how to foster a healthy and happy lifestyle.
Healthy Habits for Children
It is important to start teaching children good habits at an early age. At every developmental stage, children can benefit from learning age-appropriate ways to improve their health.
Community Well-being
Building a Healthy Community
Health is a community effort. Find out what you can do to help your community thrive by building relationships and providing resources.
WellHealthOrganic Initiatives
Learn about WellHealthOrganic’s efforts to make the world a better, more sustainable place. Become a part of the crusade for world peace.
Seasonal Well-being
Adapting Well Health Tips to Seasons
Our health is affected by the changing seasons. Optimal health is achieved when one’s lifestyle, nutrition, and routines are adjusted to align with the changing seasons.
Seasonal Foods for Well-being
Find out what’s in season so you may satisfy your taste senses while still meeting your body’s nutritional demands.
Common Health Myths
Debunking Well Health Myths
Disentangle reality from fantasy. Debunk health misconceptions so you may make well-informed decisions for your overall wellness.
Separating Facts from Fiction
Equip yourself with reliable data. The best way to take care of your health is to be knowledgeable about the science underlying good health habits.
Personalized Well-being
Tailoring Well Health Tips to Individuals
We are all special in our own way. Discover tailored health advice based on your unique requirements, tastes, and aspirations.
Bio-Individuality in Health
Recognise the uniqueness of your biomes. Learn how your individual make-up affects your health and adjust your habits appropriately.
Aging Gracefully
Well Health Tips for Seniors
Life expectancy is numeric. Get the most out of your golden years by following these health suggestions designed just for seniors.
Embracing WellHealthOrganic Aging
Learn how to age gracefully by following the concepts of WellHealthOrganic. A successful senior life may be achieved by cultivating a good outlook and healthy routines.
Technology and Well-being
Balancing Screen Time
Keeping screen time to a reasonable limit is important for health in this digital era. Learn how to keep your connection with technology positive.
Utilizing Tech for Well Health
Make use of technology to improve your health. Learn about tools, resources, and applications that can improve your health journey.
Mind-Body Connection
Understanding the Mind-Body Link
Discover the mysteries of the link between the mind and the body. Learn more about the ways in which emotional and psychological health impact physical wellness.
Practices for a Healthy Connection
Do things that help you feel better physically and mentally. Nurture a healthy relationship with mindfulness exercises and holistic therapies.
Social Well-being
Importance of Social Connections
For optimal health, human relationships are crucial. Examine the significant role that interpersonal connections have in determining one’s psychological and emotional health.
Nurturing Relationships for Well Health
Cultivate and maintain meaningful connections. Find out what it takes to build a social circle that is both helpful and beneficial to your health.
Outdoor Activities
Benefits of Outdoor Exercise
Take a walk in the park for your health. Discover the rejuvenating effects of outdoor exercise on your body and mind.
Connecting with Nature for Well-being
Lose yourself in the soothing embrace of nature. Discover the many ways in which spending time in nature may improve your health.
Conclusion
To sum up, living a healthy life is an ongoing process that may be enhanced by being proactive, adopting sustainable habits, and seeing the big picture. If you want to live a full, healthy life, embrace WellHealthOrganic living.
FAQs
Q: What are the key principles of WellHealthOrganic living?
A: WellHealthOrganic lifestyle places an emphasis on a balanced relationship between people and their natural surroundings via the adoption of organic techniques, sustainable lifestyle choices, and holistic health.
Q: How can I boost my immune system naturally?
For the best immune health, it’s important to eat foods that stimulate the immune system, drink plenty of water, get enough sleep, and keep a balanced lifestyle.
Q: Is mindful eating effective for weight management?
Yes, practicing mindful eating may help with weight control in three ways: by making us more aware of our eating patterns, by helping us develop a healthy connection with food, and by keeping us from overeating.
Q: What are some practical stress-relief techniques?
A: Mindfulness meditation, deep breathing exercises, exercise, and partaking in enjoyable hobbies or pastimes are all great ways to relieve stress.
Q: How can I promote well health in my community?
An answer would be to help the community as a whole by planning wellness activities, making new friends, and donating to causes that are already working to improve people’s health and the environment.
Q: Are there specific well health tips for seniors?
A: Older adults may put their health first by engaging in regular physical activity, eating a healthy, well-balanced diet, making and keeping friends, and adopting other positive ageing habits.
-

 Social Media10 months ago
Social Media10 months agoWho is Rouba Saadeh?
-

 Apps10 months ago
Apps10 months agoWhy is Everyone Talking About Hindi Keyboards?
-

 Social Media10 months ago
Social Media10 months agoMati Marroni Instagram Wiki (Model’s Age, Net Worth, Body Measurements, Marriage)
-

 Entertainment10 months ago
Entertainment10 months ago12 Online Streaming Sites that Serve as Best Alternatives to CouchTuner
-
 Apps10 months ago
Apps10 months agoThings you need to know about Marathi keyboard today
-

 Apps10 months ago
Apps10 months agoStuck with Your default Bangla keyboard? Isn’t it time for a change?
-
 Entertainment10 months ago
Entertainment10 months agoMovierulz Website: Movierulzz 2021 Latest Movies on Movierulz.com
-

 Social Media10 months ago
Social Media10 months agoBrooke Daniells: Everything About Catherine Bell’s Partner
